(410) 764-7044
6506 Reisterstown Road, Baltimore
1205 York Road, Lutherville
6305 Belair Road, Baltimore
7809 Wise Avenue,
Dundalk

Causes and Risk Factors of Cracked Heels

Cracked heels, medically known as heel fissures, occur when the skin around the heel becomes dry, thickened, and eventually splits. This common foot condition can cause discomfort, pain, and even bleeding in severe cases. Several factors contribute to cracked heels, including prolonged standing, walking barefoot, wearing open-back shoes, and dry weather conditions. Individuals with naturally dry skin or certain medical conditions such as diabetes or thyroid disorders are at a higher risk of developing cracked heels. Additionally, factors like obesity, dehydration, and poor foot hygiene can exacerbate the problem. The lack of moisture and exfoliation leads to the build-up of dead skin, creating pressure on the heels and increasing the likelihood of cracking. Prevention is important, and this can be achieved by maintaining proper foot hygiene, moisturizing regularly, wearing appropriate footwear, and avoiding prolonged standing. If you have developed cracked heels, it is suggested that you schedule an appointment with a podiatrist who can prescribe the necessary treatment for relief.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Plaza Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Solutions for Cracked Heels
Cracked heels can make life very frustrating and embarrassing when displaying the bare feet. Aside from being unpleasing to the eye, they can also tear stockings and socks and wear out shoes at a faster rate. When severe, cracked heels may cause pain or infection.
Cracked heels are a problem for those who are athletic, those who may walk a lot, and those who have especially dry skin. Those who use medication that dry the skin, those who swim often, wearing certain types of shoes, and those who are diabetic may have trouble with cracked heels. Seniors whose skin produces less oil may also have trouble with cracked feet. There is no one way to develop cracked feet, and there is no cure.
Today, the market consists of numerous products that have a variety of ingredients to promote healing. Some of these are over-the-counter. Others are prescribed by a doctor, especially for those who have chronic dry feet and heels.
Some doctors recommend wearing socks at night for those with rough skin. This helps further healing, and helps creams stay on longer and better absorb into the skin.
One way to alleviate dryness that causes cracked heels is by using moisturizers both day and night. Another way is to make sure the skin is clean and dry at all times. Using a pumice stone to buff away dead skin before putting on moisturizer can also help. Cracked heels will not respond to the cream unless the outer layer of skin is first removed through exfoliation. After exfoliation, lotion or ointment will be absorbed by the skin more easily.
Foods that produce healing and balance can also help the skin from within. Everything that is put into the body can either help it or hurt it. Taking supplements of omega-3 fatty acids and zinc can also be very beneficial.
Nevertheless, not all products are guaranteed to help treat cracked feet. Seeing a professional is best if other treatments options were unsuccessful. A podiatrist should be able to give the best advice to help with this problem.
Bunion Formation

Bunions are bony protrusions at the base of the big toe, and manifest gradually due to a combination of genetic predisposition and external factors. Inherited structural foot issues, such as flat feet or low arches, contribute to the vulnerability of developing bunions. The gradual shifting of the metatarsophalangeal joint creates misalignment, causing the big toe to lean towards the other toes. Wearing ill-fitting footwear, particularly shoes with narrow toe boxes, exacerbates this condition by squeezing the toes together. High heels further elevate the risk, tilting the body weight forward and putting added pressure on the joint. Over time, these repeated stresses lead to the development of bony growths. Additionally, inflammatory conditions such as arthritis can accelerate bunion formation. Many bunions are unsightly and uncomfortable. If you have developed a bunion, it is suggested that you consult a podiatrist who can determine what the best treatment method is for you, which may include surgery for permanent removal.
If you are suffering from bunion pain, contact one of our podiatrists of Plaza Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Facts About Pronation of the Feet
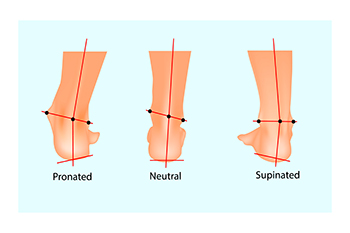
Understanding the intricacies of pronation is essential for runners, as it significantly influences shock absorption and the efficiency of push-off during each stride. Pronation, which is simply the natural side-to-side movement of the foot, comes in three main types. Normal or neutral pronation, where the foot rolls naturally inward by approximately15 percent, ensures proper shock absorption and alignment of ankles and legs. Underpronation, or supination, occurs when the foot rolls outward. This is more common among people with higher arches and can lead to injuries like Achilles tendonitis and shin splints. Overpronation involves excessive inward or downward rolling of the foot and is often associated with flat feet. Determining your pronation type is helpful for selecting appropriate footwear, but more importantly, this knowledge can minimize the risk of injuries. A podiatrist can analyze your gait and determine which type of pronation you have, factors that can result in an injury-free and a more enjoyable running experience. For a full assessment, it is suggested that you schedule an appointment with a podiatrist.
If you have any concerns about your feet, contact one of our podiatrists from Plaza Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Biomechanics in Podiatry
Podiatry is a branch of medicine that deals with the study, diagnosis, and treatment of foot and ankle conditions. There are various subdivisions in podiatry; biomechanics is one of them. Biomechanics is the way in which the bones, muscles, and joints of the feet and lower limb interact with each other.
Our feet play crucial roles in the way we move, and it is rare to have feet that are completely symmetrical. Common biomechanical issues include high or low arches or uneven leg heights. Excessive pronation often leads to fallen arches, or flat feet, and is a common cause of running injuries. People whose feet are over-pronated tend to have flexible and unstable feet. Pain is usually experienced during walking and running.
At times, people may be able to adapt to these abnormalities without any difficulties, but in other cases, these issues can cause a great deal of pain. This pain occurs because the joints, muscles, ligaments, and tendons are put under an excess amount of stress during movement. Common symptoms of biomechanical problems stemming from the feet include hip pain, knee pain, leg cramps, ankle pain, lower back pain, weak ankles, tripping, heel pain, Achilles pain, and shin splints.
Many biomechanical issues can be treated with orthotics. Orthotics are shoe insoles that are used to help control the way the foot operates. They can provide relief from foot pain, heel pain, and knee pain. Depending on your specific case, you may need to purchase over-the-counter orthotics or custom orthotics to fit your feet. Your podiatrist will be able to prescribe the perfect orthotic for your feet to help you walk around with ease.
Gait is defined as the way we move our bodies from one point to another. This is usually done by either walking or running. Gait analysis is a method used to assess the way we walk or run to highlight biomechanical abnormalities. Gait analyses are a great way to take a detailed look at how you walk and how your foot moves while you walk. An examination of the feet will help your podiatrist understand why you are suffering pain in other parts of your body.
Development of Foot Corns and Calluses

Corns and calluses are thickened skin areas caused by pressure, often occurring on the feet. They result from a natural skin defense mechanism called hyperkeratosis. Calluses are flat and spread out, while corns are thick, localized, and can have a conical shape. Corns may appear dry or translucent and are also known as helomas or clavi, while calluses are called tylomas. Common areas for corns to develop can include the sole of the foot, the outside of the pinky toe, and between the 4th and 5th toes. Corns between the toes are termed soft corns, while those in other locations are hard corns. Hyperkeratosis occurs when the skin thickens due to friction or pressure, often related to foot deformities, wearing tight shoes, or abnormal walking patterns. Risk factors include foot anatomy, gait issues, bunions, ill-fitting shoes, and certain occupations. If you have a corn or callus that becomes bothersome or shows signs of infection, it is suggested that you seek the counsel of a podiatrist who can examine the area, provide treatment for relief, and help you find underlying causes for their development.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact one of our podiatrists of Plaza Podiatry. Our doctors will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
- Wearing properly fitting shoes that have been measured by a professional
- Wearing shoes that are not sharply pointed or have high heels
- Wearing only shoes that offer support
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Corns and Calluses
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.
Triggers of Plantar Warts

Plantar warts, small growths caused by the human papillomavirus, or HPV, are notorious for cropping up on the soles of the feet, bringing discomfort and annoyance. Understanding the triggers behind their occurrence is essential for prevention. The virus thrives in warm, moist environments, making communal spaces like swimming pools, locker rooms, and public showers prime breeding grounds. Walking barefoot in these areas increases the risk of viral exposure. Additionally, cuts or abrasions on the soles create entry points for the virus, facilitating infection. Weakened immune systems, often seen in individuals under stress or with underlying health conditions, make them more susceptible to plantar warts. While direct contact with the virus is the primary mode of transmission, the virus can also be contracted indirectly through contaminated surfaces. Awareness of these triggers empowers individuals to adopt preventive measures, such as wearing protective footwear in public areas and maintaining foot hygiene, to thwart the onset of plantar warts. If you have developed a plantar wart, it is suggested that you consult a podiatrist who can offer the treatment method that is best for you.
Plantar warts can be very uncomfortable. If you need your feet checked, contact one of our podiatrists from Plaza Podiatry. Our doctors will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.