(410) 764-7044
6506 Reisterstown Road, Baltimore
1205 York Road, Lutherville
6305 Belair Road, Baltimore
7809 Wise Avenue, Dundalk

Toe Pain
Toe pain can originate from corns, calluses, hammertoes, and bunions, as well as ingrown toenails, sprains, fractures, and dislocations. Corns develop as the toe rubs against the inside of a shoe which causes the skin to thicken as a form of protection. A corn is typically cone-shaped and has a small, hardened spot that points inward. When a corn is pressed into the skin, the toe becomes painful. Corns usually form on the top or side of the toe. A callus is also a thickened patch of skin that generally forms on the bottom of the foot. Calluses are the result of friction from the toe rubbing against the inside of a shoe. They may also occur by walking barefoot or having flat feet. A hammertoe is a bump on the knuckle of the second toe that is produced by wearing shoes that are too short for your feet. The bony protrusion rubs against the top of the shoe causing pain and irritation. A bunion is a malformation of the big toe. The base of the big toe pushes away from the smaller toes, forcing the top of the big toe to press toward the other toes. Bunions can be hereditary, or they can result from injury to the toe joint or from wearing high heels with a narrow toe box. The toe becomes inflamed, and a bump may develop at the end of the misplaced bone. Ingrown toenails typically affect the big toe and its surrounding skin. The nail will dig into the skin and become painful. Wearing tight or narrow shoes that compress the big toe causes the nail to grow into the fleshy part of the toe. Cutting toenails incorrectly can also add to the development of an ingrown toenail. A toe sprain originates from a torn or stretched ligament. Strapping the injured toe to the toe next to it for stabilization is common. A broken or fractured toe usually occurs from trauma like dropping a heavy object on it or bumping into something extremely hard and rigid. Osteoporosis, a thinning of the bones, can also bring about toe fractures.
Any of the conditions mentioned can lead to pain and irritation. While some are more serious than others, seeking an examination and diagnosis from a podiatrist is a good idea. A podiatrist can treat each ailment and get you back on your feet again without pain.
Causes and Risk Factors of Ingrown Toenails

An ingrown toenail develops when the nail grows into the surrounding skin, causing pain, swelling, and potential infection. The big toe is the most common site of an ingrown toenail, and improper nail trimming is a leading cause. Cutting the toenails too short or rounding their edges can encourage the nail to grow into the skin. Wearing tight shoes, repetitive pressure from physical activities, and excessive sweating can also increase the risk. Some people have naturally curved or thick nails that make them more prone to this condition. Ingrown toenails are more common in teenagers and young adults, with males affected more often than females. If left untreated, an ingrown toenail can become infected, making daily activities difficult. A podiatrist can provide treatment, including lifting the nail, trimming properly, or surgery to remove part or all of the affected nail. Proper footwear and trimming nails straight across can help to prevent recurrence. If you have a painful ingrown toenail, it is suggested that you schedule an appointment with a podiatrist for an exam and appropriate treatment options.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact one of our podiatrists of Plaza Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Sedentary Foot Pressure and Immobility in Seniors

Prolonged inactivity may impose unintended pressure across various regions of the foot, leading to discomfort and reduced mobility. When one remains sedentary, muscles weaken and tissues lose resilience, causing abnormal weight distribution on the plantar surface. This uneven pressure is often concentrated beneath the heel, midfoot, and forefoot, resulting in callus formation and inflammation. Over time, restricted movement may compromise blood flow and nerve sensitivity, further aggravating foot pain and stiffness. These cumulative effects not only hinder everyday activities but also risk accelerating immobility. Integrating gentle stretching and regular exercise can mitigate these adverse outcomes while reinforcing natural foot mechanics. Regular movement not only alleviates pressure but also fosters significantly improved circulation and overall foot strength. For any persistent foot pain or emerging complications, it is strongly suggested that you consult a podiatrist for a comprehensive evaluation and advice tailored to your needs.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with one of our podiatrists from Plaza Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Foot Pain
The feet, being the foundation of the body, carry all of the body’s weight and are therefore prone to experiencing pain and discomfort. If you are experiencing foot pain, it is important to determine where in the foot you are experiencing this pain to help discover the cause of it. While pain can be experienced virtually anywhere in the foot, the most common sites of foot pain are in the heel and ankle.
Heel pain can be due to a multitude of conditions including plantar fasciitis, Achilles tendinitis, and heel spurs. Pain experienced in the ankle can be a sign of an ankle sprain, arthritis, gout, ankle instability, ankle fracture, or nerve compression. In more serious cases, pain in the foot can be a sign of improper alignment or an infection.
Foot pain can be accompanied by symptoms including redness, swelling, stiffness and warmth in the affected area. Whether the pain can be described as sharp or dull depends on the foot condition behind it. It is important to visit your local podiatrist if your foot pain and its accompanying symptoms persist and do not improve over time.
Depending on the location and condition of your foot pain, your podiatrist may prescribe certain treatments. These treatments can include but are not limited to prescription or over-the-counter drugs and medications, certain therapies, cortisone injections, or surgery.
If you are experiencing persistent foot pain, it is important to consult with your foot and ankle doctor to determine the cause and location. He or she will then prescribe the best treatment for you. While milder cases of foot pain may respond well to rest and at-home treatments, more serious cases may take some time to fully recover.
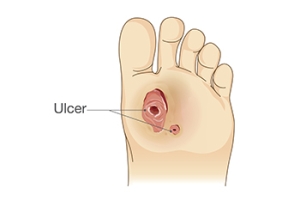
Finding Relief From Foot Ulcers
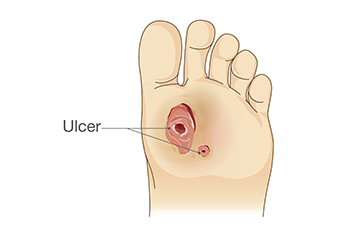
A foot ulcer is an open wound that develops on the bottom of the foot, often affecting individuals with diabetes or poor circulation. These ulcers are typically caused by nerve damage, prolonged pressure, and poor blood flow, which slow down the body’s natural healing process. Symptoms include pain, redness, swelling, and sometimes drainage or a foul odor, particularly when the ulcer becomes infected. Keep the wound clean and dry, and avoid putting pressure on the affected area for mild relief. Wearing proper footwear and using padded insoles can also help reduce pressure. If you have a foot ulcer, it is strongly suggested that you are under the care of a podiatrist who can treat foot wounds and help you manage any contributing underlying condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with one of our podiatrists from Plaza Podiatry. Our doctors will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
How Fibromyalgia Affects the Feet

Fibromyalgia can cause persistent foot pain, often affecting the heels, arches, toes, and ankles. This chronic disorder heightens sensitivity in the nervous system, making weight-bearing activities uncomfortable. Many patients experience aching, burning, or stabbing sensations in their feet, which can fluctuate in intensity. Stiffness, swelling, and tenderness are also common, particularly in the morning or after prolonged standing. Poor circulation, common in fibromyalgia, may contribute to cold feet or a tingling sensation. Wearing ill-fitting shoes or prolonged pressure on the feet can worsen symptoms, making everyday movement difficult. While fibromyalgia does not directly damage the foot’s structure, ongoing pain and discomfort can alter walking patterns, leading to strain in the ankles and an increased risk of imbalance. A podiatrist can assess your foot mechanics, recommend supportive footwear, and provide custom orthotics to ease discomfort. They may also suggest additional treatments to improve mobility and alleviate pain. If you have foot pain connected to fibromyalgia, it is suggested that you schedule an appointment with a podiatrist for treatment options.
When dealing with systemic disease of the feet, it is extremely important to check the affected areas routinely so that any additional problems are caught quickly. If you have any concerns about your feet and ankles contact one of our podiatrists from Plaza Podiatry. Our doctors will assist you with all of your podiatric needs.
Systemic Diseases of the Feet
Systemic diseases affect the whole body, and symptoms usually are displayed in the feet. This condition can make a patient’s ability to walk unbearable. Systemic diseases include gout, diabetes mellitus, neurological disorders, and arthritis.
Gout – is caused by an excess of uric acid in the body. Common symptoms include pain, inflammation, and redness at the metatarsal/phalangeal joint of the base big toe. Gout can be treated by NSAIDs to relieve pain and inflammation, and other drugs that lower the acid levels in the body.
Diabetes mellitus – is an increase in the level of blood sugar that the body cannot counteract with its own insulin. Failure to produce enough insulin is a factor in Diabetes.
Diabetes of the Feet
Diabetic Neuropathy – may lead to damaged nerves and affect the feet through numbness and loss of sensation.
Peripheral Vascular Disease – can restrict the blood flow to the feet, and often times lead to amputation of the feet.
If you have any questions please feel free to contact our offices located in Baltimore, Lutherville, and Dundalk, MD . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Systemic Diseases of the Foot
There are several systemic diseases, or diseases that affect the whole body, that either display symptoms in the feet or affect the health of the feet. Common systemic diseases that affect the overall health of the feet, and the patient’s ability to walk comfortably, include gout, diabetes mellitus, neurological disorders, and arthritis, among others.
In gout, which is caused by an excessive buildup of uric acid in the body, the most common symptoms of pain, inflammation, and redness occur at the metatarsal/phalangeal joint at the base of the big toe. Any excess levels of uric acid crystallize and are deposited in tendons, joints, and surrounding bone and muscle tissue. Gout is commonly treated with NSAIDs to relieve pain and inflammation and other drugs to lower uric acid levels in the body. Gout most commonly affects those who are overweight, have low protein diets and lead a more sedentary lifestyle.
Diabetes mellitus is an increase in the level of blood sugar in which the body cannot counteract with naturally occurring insulin in the body. The three types of diabetes, Type I, Type II and Gestational Diabetes, are all signs the body is either not producing enough insulin or is not efficiently using the insulin that is produced. Gestational diabetes only affects women who are pregnant and have never, prior to pregnancy, exhibited symptoms of the disease.
There are two main issues that affect the feet that are commonly caused by diabetes. They include diabetic neuropathy and peripheral vascular disease. Diabetic neuropathy can lead to damaged nerves and affect the feet through numbness and loss of sensation. Peripheral vascular disease restricts the flow of blood to the foot and can, in extreme cases, lead to the necessity of amputating the foot. Peripheral issues that are caused by diabetes and can affect the foot include athlete’s foot, nail infections, corns, blisters, bunions, severe dry skin, plantar warts and ingrown toenails. These can all be attributed to the decrease of blood flow to the foot.
Neurological disorders and rheumatoid arthritis can also have severe impact on the health of the feet. Neurological disorders can affect the nerves in the main structure of the foot and cause loss of sensation and possible decreased muscle response. Rheumatoid arthritis can affect the bones and joint structures of the foot, making it impossible to walk normally without serious pain.
All systemic diseases that affect the foot can effectively be treated to minimize joint and muscle damage if they are diagnosed early and treated with medication and lifestyle therapy. Diabetes patients must monitor their blood sugar levels and work with their physician to keep their levels as close to normal as possible. Rheumatoid arthritis patients should work with their physician to ensure the proper medications are being taken to reduce the amount of damage to the joints of the body.